Nursing roles in diabetes management.
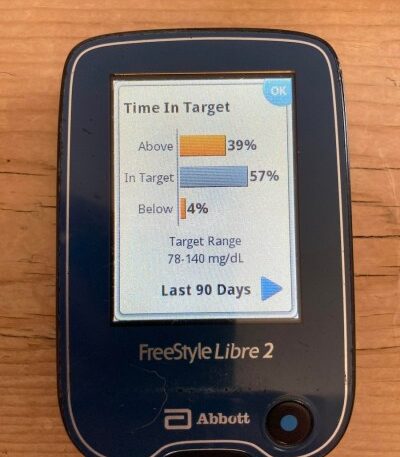
A continuous glucose monitor reader (or a smartphone app) scans the sensor attached to the patient’s body for interstitial fluid glucose level and can provide data such as average blood glucose level or percentage of time spent in a target range over a given period of time.
Knowledge is power. When a person with diabetes knows their blood glucose levels, they can better self-manage lifestyle choices and medications and be an active participant in preventing complications. Glucose information can be obtained through a variety of methods. The majority of people with known diabetes receive reports on their glucose from the health care provider who is able to do lab work to obtain fasting or random blood glucose level, hemoglobin A1c (HbA1c, or just A1c) level, and urine glucose.
Nurses play an integral role to partner with the patient about their diabetes and provide education on the meaning of glucose measurement. In the outpatient setting, nurses can help the patient adjust insulin dosages and work on glucose monitoring skills and interpretation. Inpatient, nurses oversee and utilize glucose results and help with self-management skills in anticipation of care at home or by family.
Limitations of capillary blood glucose monitoring.
Blood glucose checks are done at a specific time of day such as fasting, before a meal, two hours after a meal, bedtime, and when symptoms of low or high glucose are present. However, glucose meters analyzing a drop of blood obtained via finger stick return a blood glucose value but do not indicate the direction of the glucose, whether stable, rising, or descending. In addition, many patients perform these glucose checks only intermittently if at all, either because of lack of access to monitoring equipment, inability to perform the glucose check, not knowing what to do with the result, or problems with affordability.
The A1c test.
The hemoglobin A1c test examines red blood cells to provide a value that reflects the average blood glucose for the previous three months. The A1c is a standard glucose measurement of control and over time can help predict risk of diabetes complications. While the A1c is a great tool, it works best in combination with intermittent home glucose monitoring.
The A1c will continue to be used to determine if a patient’s average glucose level meets an established goal, but a major limitation of the A1c is that it does not reveal history of hyperglycemia and hypoglycemia. Since the A1C is only an average, the person with diabetes and their clinician do not know whether the average glucose level results from relatively stable blood glucose levels within a target range during this period or whether it reflects an average that includes many highs and lows. Ideal control would mean maintaining a steady glucose level with few extremes of glucose that can be dangerous, distressing to the person with diabetes, and indicate areas for improvement in glucose self-management.
Positives of continuous glucose monitoring.
Now that continuous glucose monitoring (CGM) is available, this form of monitoring is especially helpful for people with type 1 diabetes who need to adjust insulin dosages frequently to account for activity and quantity of carbohydrates eaten. It is also useful for revealing which times of day glucose is better or less well controlled. People with type 2 who are on insulin, have widely variable glucose levels, or need to alter medication dosages may also benefit from CGM use. Medication adjustment is much easier for both patient and clinicians when data beyond an average or a single point in time is available.
An additional benefit of the CGM is that it has alarms to alert the user about pending and actual hypo- and hyperglycemia. The alarms are particularly crucial in people who have difficulty recognizing potentially dangerous low blood glucose.
CGMs can measure ‘time in range.’
Use of CGMs has made an additional measure of glucose control possible. The measure is time in range (TIR), which is the amount of time or percentage or time that the glucose is within the goal range over a given period. Ideally, glucose is in range at least 70% of the time. Pre-meal glucose target range for non-pregnant adults with diabetes is usually 80-130 mg/dl (3.9-10 mmol/l), but the goals can be individualized based on needs or lowered based on age and risk.
Applying the data.
CGM data with percentages of time in range and graphs can be reviewed by the person with diabetes and the health care provider for detailed interpretation and treatment guidance. Research has shown that time in range offers information that, together with the A1c level, gives patients the potential for better knowledge, better control, and ultimately fewer complications.
With a difficult disease that requires so much self-management, effective tools like CGMs and knowledgeable nurses as care providers can increase motivation and make the heavy task of glucose control manageable.
By Susan Renda DNP, ANP-BC, CDCES, FNAP, FAAN, associate professor, associate director DNP Advanced Practice Program, Johns Hopkins University School of Nursing; srenda1@jhu.edu
The post Continuous Glucose Monitoring and Time in Range: Improving Data for Diabetes Management appeared first on Off the Charts.